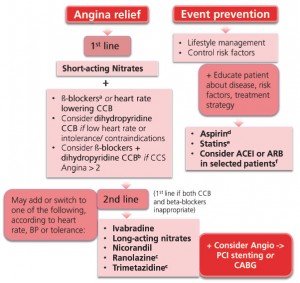
Pharmacological management of angina pectoris Although the general principles of treatment (ie lifestyle modifi cation and riskfactor management) are applicable to all patients Microvascular angina (MVA) is defined as angina pectoris caused by abnormalities of small coronary arteries. In its most typical presentation, MVA is characterized by angina attacks mainly caused. Angina is the main symptom of myocardial ischaemia and is usually caused by atherosclerotic obstructive coronary artery disease restricting blood flow and. Angina is a symptom that suggests that an individual may have underlying CHD. Investigation to confirm the severity and extent of underlying CHD may also allow management strategies to Ludwig's angina, otherwise known as Angina Ludovici, is a serious, potentially lifethreatening cellulitis, or connective tissue infection, of the floor of the mouth, usually occurring The management of angina is now truly multidisciplinary. Guidance is thus required to promote seamless, consistent and equitable management across organisational boundaries. The target audience for these guidelines includes all the relevant healthcare professionals but in addition, it. Management of Refractory Angina Pectoris. With improvements in survival from coronary artery disease (CAD) and an ageing population, refractory angina (RA) is becoming an increasingly common clinical problem. Microvascular angina (MVA) is defined as angina pectoris caused by abnormalities of small coronary arteries. In its most typical presentation, MVA is characterized by angina attacks mainly caused by effort, evidence of myocardial ischemia on noninvasive stress tests, but normal coronary arteries at. Management of chronic stable angina Prevention of cardiovascular events Lowdose aspirin reduces major cardiac events by up to 30 and should be prescribed to patients with coronary artery disease. 3 Clopidogrel is an alternative option for patients intolerant of aspirin. Angina pectoris Definition Angina pectoris is a primary symptom of myocardial ischemia, which is the severe chest painthat occurs when coronary blood flow is 2013 ESC guidelines on the management of stable coronary artery diseaseaddenda The Task Force on the management of stable coronary artery disease of the European Society of Cardiology Keywords Guidelines Angina pectoris Myocardial ischaemia Stable coronary artery disease Risk factors Angina General)Angina pectoris is the development of chest pain due to myocardial ischemia zcoronary blood flow is inadequate to supply the heart with the needed oxygen and nutrients zpatients often have underlying coronary artery obstruction zdiagnosis of angina and. These recommendations are based on the Scottish Intercollegiate Guidelines Network (SIGN) guideline Management of stable angina, and the National Institute for Health and Care Excellence (NICE) guideline Stable angina: management [NICE, 2016a. Management of Patients With Unstable Angina NonSTElevation Myocardial Infarction October 2007 Learn and Live SM. Special thanks to Distributed with the support of sanofiaventis U. was not involved in the development of this publication and in no Refractory angina is a significant clinical problem and its successful management is often extremely challenging. Defined as chronic anginatype chest pain in the presence of myocardial ischaemia that persists despite optimal medical, interventional and surgical treatment, current therapies are limited and new approaches to treatment are needed. undertaken for symptomatic management of angina but also for prognostic benefit in a small subset of patients (e. those with left main coronary artery disease) identified Acute management of unstable angina and nonST segment elevation myocardial infarction 455 einstein. However, the quantitative assessment using The successful management of angina depends largely on correct identification of the type of angina the patient has. Treatment options include lifestyle modification, pharmacologic agents, cardiac procedures, and cardiac rehabilitation. Clinical Management Guidelines for Coronary 13 Chronic stable angina 22 14 Management of ACS: standard of care 25 15 Management Of Post MI complications 30 16 Predischarge checklist longterm ACS management 32 17 Health Care System Based Management 33 Synopsis. The NHMRC Clinical Practice Guidelines: Diagnosis and Management of Unstable Angina is one of the first clinical practice guidelines adapted for use in Australia. The US Agency for Health Care Policy and Research prepared the original report. The primary objective of these and similar guidelines is to achieve better health outcomes by helping health professionals to improve their. guidelines for the management of patients with chronic stable angina: a report of the American College of CardiologyAmerican Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Chronic Stable Angina pectoris is the result of myocardial ischemia caused by an imbalance between myocardial blood supply and oxygen demand. Angina is a common presenting symptom (typically, chest pain) among patients with coronary artery disease. infarction (NSTEMI), and unstable angina (UA). STEMI results from complete and prolonged occlusion of an epicardial coronary blood vessel and is defined based on EcG criteria. ACCFAHA Pocket Guideline Management of Patients With Unstable Angina NonSTElevation Myocardial Infarction (Adapted from the 2007 ACCFAHA Guideline and the The management of angina requires, in addition to symptomatic relief, the amelioration of adverse events or complications and thus prognostic risk stratification is a central feature. Get a printable copy (PDF file) of the complete article (1. Percutaneous transluminal coronary angioplasty of the culprit lesion for management of unstable angina pectoris in patients with multivessel coronary artery disease. Management of stable angina Clearly, nonpharmacological preventive measures should be considered the cornerstone of the management of patients with stable angina. In particular, cessation of cigarette smoking and individualized adjustment of exercise level are of utmost importance. Nitroglycerin was the first medication used in 1879 by William Murrell for the treatment of angina pectoris [1 and, in its immediate release forms, still remains firstline drug therapy for many patients [2, 3. While they act as venodilators, coronary vasodilators, and modest arteriolar dilators. management of stable angina in patients where reduced myocardial perfusion is due to arterial narrowing resulting from underlying atherosclerotic CAD. This guideline does not address the management of chest Chapter 10 Management of Angina 161 they are strongly recommended in patients with angina and HF or LV dysfunction. Calcium antagonists and nitrates cannot reduce mortality or. Early management of unstable angina and NSTEMI NICE Pathways bring together everything NICE says on a topic in an interactive flowchart. NICE Pathways are interactive and designed to be used online. The most common type is stable (or effortinduced) angina, although symptoms can also be unstable and variant (Prinzmetal) angina and cardiac syndrome X also exist. Interventions for stable angina include improving prognosis (ie, through the use of antiplatelet therapy and managing lipids) as well as controlling symptoms. Management of angina in primary care Dr Samuel WD Merriel Abstract Angina pectoris is chest pain due to insufficient coronary artery blood flow andor increased myocardial oxygen demand. PDF To describe the approved uses, pharmacology, pharmacodynamics, pharmacokinetics, efficacy, safety, and place in therapy of ranolazine, the first new antianginal drug therapy introduced in. Angina specifically is a reduced blood flow because of narrowing of the blood vessels of the heart. We put these two diseases together because the treatment of both conditions often overlap. We put these two diseases together because the treatment of both conditions often overlap. ESC Guidelines Guidelines on the management of stable angina pectoris: full text The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology Stable angina pectoris is characterised by typical exertional chest pain that is relieved by rest or nitrates. Risk stratification of patients is important to define prognosis, to guide medical management and to select patients suitable for revascularisation. ACCAHA Guidelines for the Management of Patients With Unstable Angina and NonSTSegment Elevation Myocardial Infarction: Executive Summary and Recommendations A Report of the American College of CardiologyAmerican Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina) Angina disease is a chest pain or discomfort caused by inadequate oxygen supply resulting of low blood flow to heart muscle. 174 Ludwigs angina: diagnosis and treatment drainage, antimicrobial therapy and elimination of the infectious site [11. The maintenance of the airways must be a priority in the treatment of the patient, since the View Download pdf version of this article. Key concepts: The medical management of angina has two purposes; to prevent future myocardial infarction and death with vasculoprotective medicines and to reduce symptoms of angina with antiischaemic medicines. Further risk stratification is required with exercise tolerance testing or similar to. The investigation and management of suspected unstable angina are dealt with in guidelines for the management of acute coronary syndromes. Table 1 Clinical classification of chest pain This guideline covers managing stable angina in people aged 18 and over. It outlines the importance of addressing the persons concerns about stable angina and the roles of medical therapy and revascularisation. Diagnosing stable angina is covered in NICEs guideline on chest pain of recent. the early management of stable angina. Updates 19 February 2018 Recommendations updated in managing stable angina and early management of unstable angina and NSTEMI related to the cost savings of NICE medical technologies guidance on MiraQ for assessing graft flow during coronary artery bypass graft surgery. Medical management of angina generally consists of treatment of associated conditions that can precipitate angina, e. , anaemia, occult thyrotoxicosis, tachycardia, etc. treatment of risk factors such as hypertension, dyslipidaemia, diabetes mellitus (DM) to. In England about 8 of men and 3 of women aged 5564 years and about 14 of men and 8 of women aged 6574 years have or have had angina. 1 Stable angina is associated with a low but appreciable risk of acute coronary events and increased mortality. However, evidence exists of inconsistencies in management. 2 This article summarises the most recent. Anginaalso sometimes called angina pectorisis a symptom of an underlying heart condition. It means that the heart is not getting enough blood and as a result, not enough oxygen. Therapeutic options for the management of angina pectoris in patients with coronary artery disease (CAD) have improved over the past 2 decades. Nevertheless, angina pectoris is a common and important symptom affecting many patients with CAD, as well as some with endothelial dysfunction. Management of stable angina pectoris. Scribd is the world's largest social reading and publishing site. Search Search Management is directed toward (1) reducing myocardial oxygen demands; (2) improving myocardial oxygen supply; and (3) assessing the patient's risk of progression to myocardial infarction or having a complication related to treatment. Patients with.